BREAST RECONSTRUCTION USING TISSUE FLAPS IN HOUSTON, TX
Home » Breast Procedures » Breast Reconstruction » Tissue Flap Breast Reconstruction
Breast reconstruction is regarded as a life-changing opportunity for women who have undergone a mastectomy as a result of breast cancer. Although there is no procedure that can completely restore feeling to the breast region after a breast removal surgery, there are a number of reconstruction options available to women today to restore the appearance of their chests. For those who prefer a more natural approach to reconstruction instead of breast implants, our surgeons offer breast reconstruction using tissue flaps, a procedure also known as flap surgery or autologous reconstruction.
Flap surgery can be performed immediately after a mastectomy or at a later date. In this procedure, a portion of tissue is removed from an area of the body – usually the abdomen – and relocated to create a new breast mound that will look natural when fully healed.
Breast reshaping is a complex surgical procedure that requires the patient to be in good health prior to treatment. At Memorial Plastic Surgery, our team of board-certified plastic surgeons is highly experienced in performing many types of flap breast reconstruction techniques to ensure that the patient is satisfied with her aesthetic outcome.
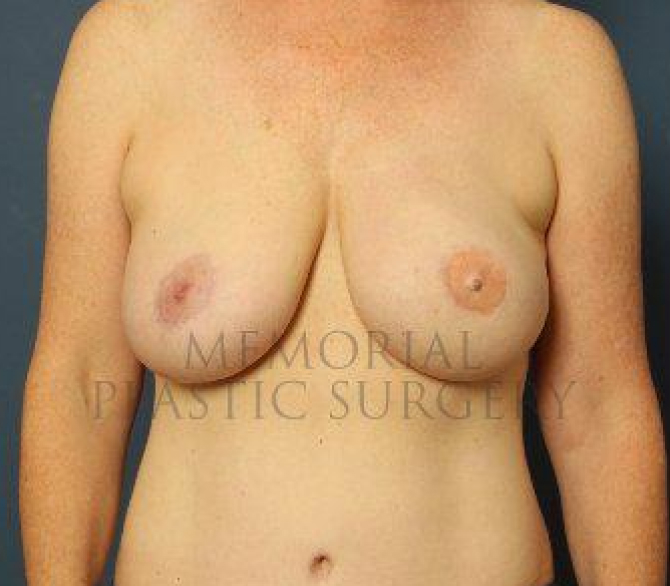

real patient DIEP Flap Surgery results
Ideal Candidates for Breast Reconstruction Using Tissue Flaps
The various techniques of breast reconstruction involve making an alteration to the patient’s blood circulation. Individuals with blood-related illnesses or who are heavy smokers are not advised to undergo this procedure. If a patient is not suited for the procedure, our doctor will discuss possible alternative solutions in detail after a thorough assessment of their overall health.
The ideal candidate for breast reconstruction with tissue flaps is anyone who:
- Has large breasts
- Has undergone radiotherapy
- Has a close mastectomy scar
- Desires a softer and more realistic result compared to an implant
- Has had a radical mastectomy
Request Your Consultation
You can request a consultation online or if you have any questions please call the office
713-633-4411.
Tissue Flap Reconstruction with MPS Top Doctors
It is highly recommended to consult with one of our board-certified physicians prior to treatment, who will thoroughly evaluate the patient’s condition and overall health to determine which technique is most appropriate to ensure a successful reconstruction and smooth recovery.
Each of the different types of tissue flap breast reconstruction techniques requires general anesthesia, and the duration of the procedure will depend on which technique is being employed by our surgeon.
During the reconstruction procedure, the surgeon will need to remove skin, fat, or sometimes muscle from the selected donor site to restore the shape of the breast. In order to keep the tissue alive, unlike skin graft, the surgeon must keep the tissue connected to its original blood vessel. The alternative solution is to cut the blood vessels and reconnect the tissue to another vessel located under the arm, or in the chest wall.
Once the procedure is complete, our surgeon carefully closes the incision with dissolvable sutures.
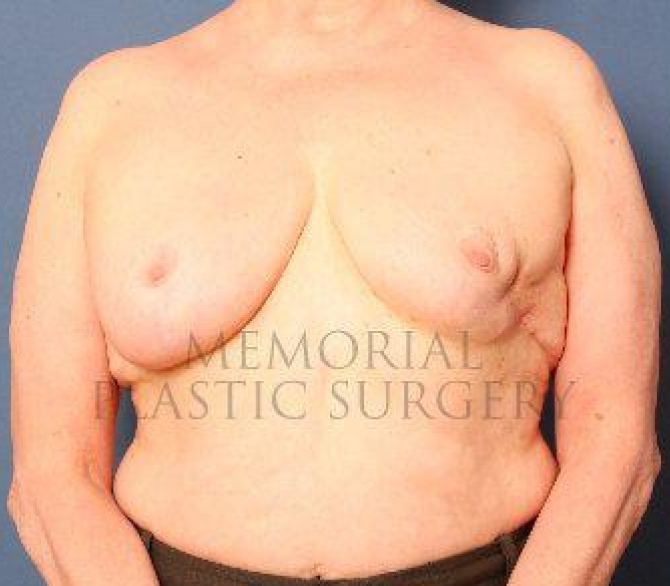

real patient Latissimus Muscle results
Different Flap Techniques
DIEP Flap
The DIEP (Deep Inferior Epigastric Perforator) flap restores the breasts using tissue, skin, and blood vessels harvested from the lower abdomen, without removing any muscle or supportive tissue in the area.
TRAM Flap
TRAM (Transverse Rectus Abdominis Muscle) flap reconstruction is a type of pedicle flap reconstruction using breast tissue harvested from the lower abdomen and away from the abdominal muscle. This is between the pubic bone and the waist, resulting in a slimmer midsection. Unlike Latissimus Dorsi flap reconstruction, TRAM flap reconstruction is best suited for patients who wish for larger breasts as this donor site has more fat tissue than the other. Our doctors perform two distinct forms of TRAM flap reconstruction procedures:
- Pedicled TRAM Flap
Recreates the breast mound by transferring the flap from the abdomen into the chest wall without separating it from its blood supply. - Free TRAM Flap
A highly advanced surgical procedure that requires incredible skill to separate the flap from its blood supply temporarily. Once the breast is restored, microsurgery is implemented to reconnect the blood vessels to the body.
SGAP Flap
Tissue is harvested from the hips and upper buttocks to create the breasts after mastectomy. The SGAP (Superior Gluteal Artery Perforator) Flap procedure is often the right choice for patients seeking to contour their bodies as it diminishes the presence of “love handles.”
IGAP Flap
The IGAP (Inferior Gluteal Artery Perforator) Flap is an option for women who may not have enough tissue in the abdomen and hips for transfer. Blood vessels, skin, and fat are harvested from the lower buttocks and transferred to the chest area using a combination of fat grafting and microsurgery.
TUG Flap
Takes tissue harvested between the groin crease and the upper inner thigh to recreate the breasts. TUG (Transverse Upper Gracilis) Flap technique is conducive to women with naturally small breasts and may not have sufficient tissue in the hips and buttocks for transfer.
PAP Flap
Uses the tissue along the profunda artery in the back of the posterior thighs to cosmetically restore the breast mound in patients who may not have enough skin and fat in other areas of the body. The blood vessels are expertly reattached using microsurgery.
Cost & Financing
Several factors may affect the total cost of the procedure, including:
- The flap technique that will be used
- Facility fees
- Anesthesia fees
- Post-operative garments
- Surgeon’s fee, which varies per doctor
The final cost of the surgery will be provided after consulting with our surgeons and once a treatment plan has been developed.
Memorial Plastic Surgery accepts all major credit cards and cryptocurrencies such as Bitcoin as payment.
Recovery & Results
After breast reconstruction with the chosen local flaps, patients are transferred to a recovery room where they are monitored for up to 5 days. Several drains are placed near the incision and are removed when fluid accumulation slows. The drains are usually removed within 1 – 2 weeks after surgery. For the first 6 weeks after surgery, patients should not lift anything that might strain the body and should not bathe for about 4 weeks.
Prior to discharge, patients will receive appropriate home follow-up instructions and prescribed pain medications to relieve pain and discomfort. Our surgeons will also fit them with a compression garment and supportive bra to support the breast during recovery, which they will need to wear for several weeks.
Although rest is the most important factor in speeding recovery, patients are encouraged to walk at home every day to promote circulation and prevent pneumonia, congestion, or blood clots.
Below is a table of expected side effects after surgery and a timeline until the patient can return to daily activities:
| POST-OP RECOVERY | ESTIMATED TIME |
| Drain use | 1 – 2 weeks |
| Wearing a supportive bra | 3 – 4 weeks |
| Compression garment use | 3 – 4 weeks |
| Physical discomfort (swelling, soreness, & bruising) | 4 – 8 weeks |
| Scar | 6 months – 1 year |
| DAILY ACTIVITIES | ESTIMATED TIME |
| Showering | 2 days |
| Resuming work / daily activities | 2 – 3 weeks |
| Heavy exercises and other strenuous activities | 4 – 6 weeks, or upon clearance by our doctor |
patient reviews
269 Reviews
“ I was extremely comfortable. He was very professional and gave great recommendations. I would defintely recommend him. ”
by Mattie W. (Verified Patient)
We schedule follow-up visits with our patients to track their healing progress. The rate of recovery is different for each patient. At these appointments with our surgeon, they will be able to determine if the prescribed medications need to be changed and if recovery is progressing so quickly that patients can resume their normal activities sooner.
Frequently Asked Questions
When can I start talking to my doctor about breast reconstruction?
If you are currently undergoing a mastectomy, you can begin to assess your options for breast reconstruction surgery. Under the guidance of your breast surgeon and a board-certified plastic surgeon, you may develop a proper surgical plan tailored based on your needs and goals
How do I know which flap reconstruction technique is right for me?
Your board-certified plastic surgeon will determine this during an initial consultation. Their assessment of your current physical condition, together with an understanding of your recent medical history, will allow them to decide which flap technique is best suited for your needs.
Which is better: tissue flap reconstruction or implant-based reconstruction?
Both approaches have their advantages and disadvantages. Ultimately, the decision between either approach will be determined by a host of factors that include your current physical health at the time of your mastectomy as well as your desired surgical outcome.
How long does it take to heal from flap surgery?
It typically takes between 1 – 2 months before your body recovers from the surgery itself. Results are immediately noticeable. However, it can take between 1- 2 years for your reconstructed breasts to settle on the chest wall.
*The content and images on this page are provided with the sole intention of educating potential patients on the procedure discussed above. Results vary per individual and are dependent on our doctor’s consultation prior to the procedure. We strongly recommend undergoing a formal consultation with a board-certified plastic and reconstructive surgeon prior to scheduling and undergoing any surgical or non-surgical treatment.